Our Research
Mucosal Immune Surveillance; Air Quality and Health
M cells and Mucosal Immune Surveillance
Mucosal surfaces in the lung and intestine are exposed to environmental antigens and allergens and, in the case of the intestine, abundant food antigens. They are also exposed to a variety of infectious organisms such as viruses (influenza, polio, SARS, HIV), bacteria (staphylococcus, streptococcus, anthrax), and parasites (Toxoplasma). The mucosal immune system must be able to identify pathogenic infectious agents and respond to them without reacting to beneficial commensal bacteria, or developing allergic responses to food or environmental antigens.
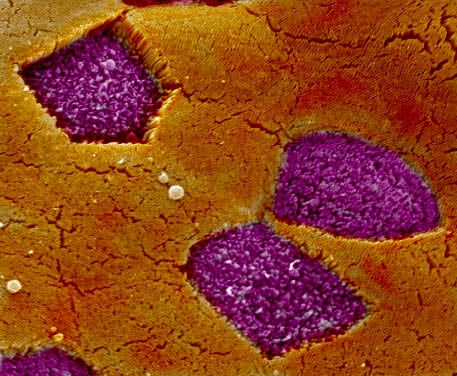
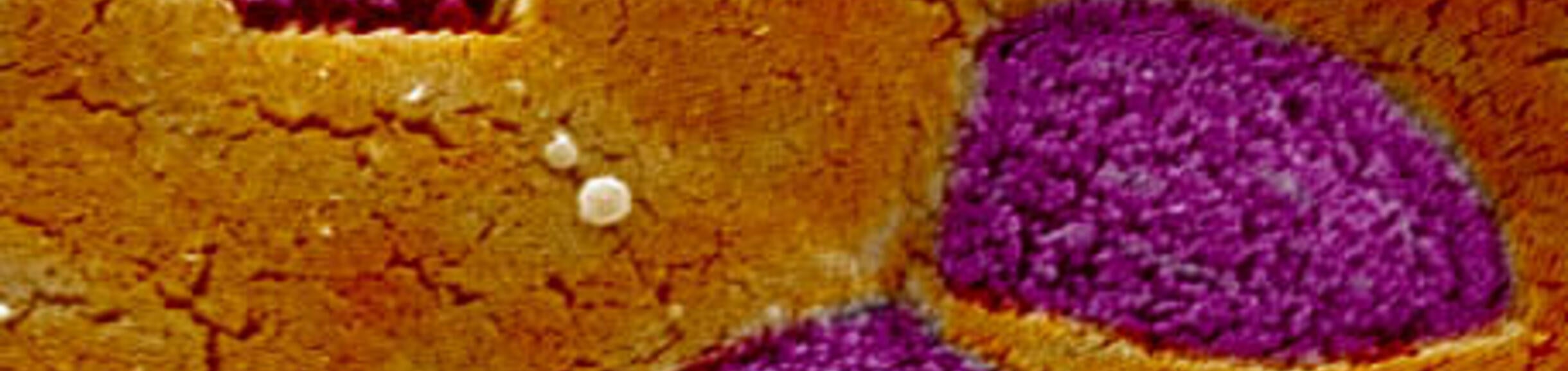
At mucosal surfaces, epithelial cells provide a tight barrier to entry into the body, but the immune system also induces the development of specialized epithelial cells called M cells to detect the presence of infectious organisms. These M cells are selective gatekeepers that capture particles such as viruses and bacteria for delivery to cells of the immune system waiting below the epithelial layer. Our laboratory has been studying the development of M cells, and the mechanisms used by M cells in their selective uptake of particles. We are also using the information we have learned about M cell function to engineer novel technologies for needle-free vaccine delivery that we hope to use against influenza and other infectious organisms. Several related projects are ongoing in our lab:
M Cell Differentiation
We have developed a cell culture model of M cell development using cytokine induction of an intestinal epithelial cell line. From gene expression profiling of this induction, we have identified genes associated with M cell function and differentiation, and signaling pathways associated with differentiation. In a gene knockout mouse model, we have also confirmed a novel signaling pathway (CD137-CD137L) necessary for the differentiation of M cells in vivo; this pathway apparently interacts with other epithelial differentiation signaling pathways. In addition, we have developed a novel transgene fluorescent reporter system for following M cell development in vivo. With this transgene we have been able to identify distinct lineages and phenotypes among M cells, and more recently, we have shown that intestinal inflammatory diseases also induce the development of new M cells in the colon. We are studying the inflammatory cytokines responsible for this induction. Our studies point to the existence of multiple M cell phenotypes, each with potentially distinct functions.
Transcytosis Machinery
We have been using confocal microscopy approaches to identifying the cellular machinery used in the endocytosis and transport of bacterial particles by intestinal epithelial cells and M cells. Interestingly, M cells may use multiple mechanisms for transporting particles across the epithelial barrier. Our studies have already identified an unusual involvement of tight junction proteins such as Claudin 4 in one important pathway of bacterial particle uptake. We also showed that M cells produce cytoplasmic microvesicles that are delivered to underlying dendritic cells, providing a novel route for delivery of intracellular antigens.
Needle-free Vaccines: M Cell-targeted Vaccine Delivery
We have identified a number of receptors used by M cells in the capture and transport of bacterial particles across the epithelial barrier. From these discoveries, we are using a variety of protein engineering approaches to develop molecular “hooks” that may be used to target the delivery of vaccine antigens to M cells; technology based on these targeting strategies has been awarded a US patent. Recombinant proteins are presently being tested as needle-free mucosal vaccine formulations that may soon have application in clinical settings. We are also designing polymer nanoparticles and biopolymer formulations as delivery vehicles for these vaccine antigens. Additional background can be found on the website of the Grand Challenges in Global Health.
Air Quality and Health
While it is well established that pollutants (e.g., diesel exhaust, ozone, etc.) have negative health effects, other exposures to environmental aerosol particulates can also have important negative health impacts. For example, in areas with high particulate counts (e.g., California's Central Valley, Coachella Valley) the environmental exposures are often associated with high rates of pulmonary inflammatory diseases such as asthma. Along with our colleagues in the BREATHE Lab, we are studying the mechanisms by which aerosolized particles induce patterns of lung inflammation. For example, we are interested in the components of dusts in the Eastern Coachella Valley that may predispose residents to develop lung inflammation, and may account for the extremely high rates of childhood asthma in the region.